
Atrial Fibrillation
Atrial fibrillation is an electrical abnormality in the heart. It affects the way the electrical wiring in the heart works.
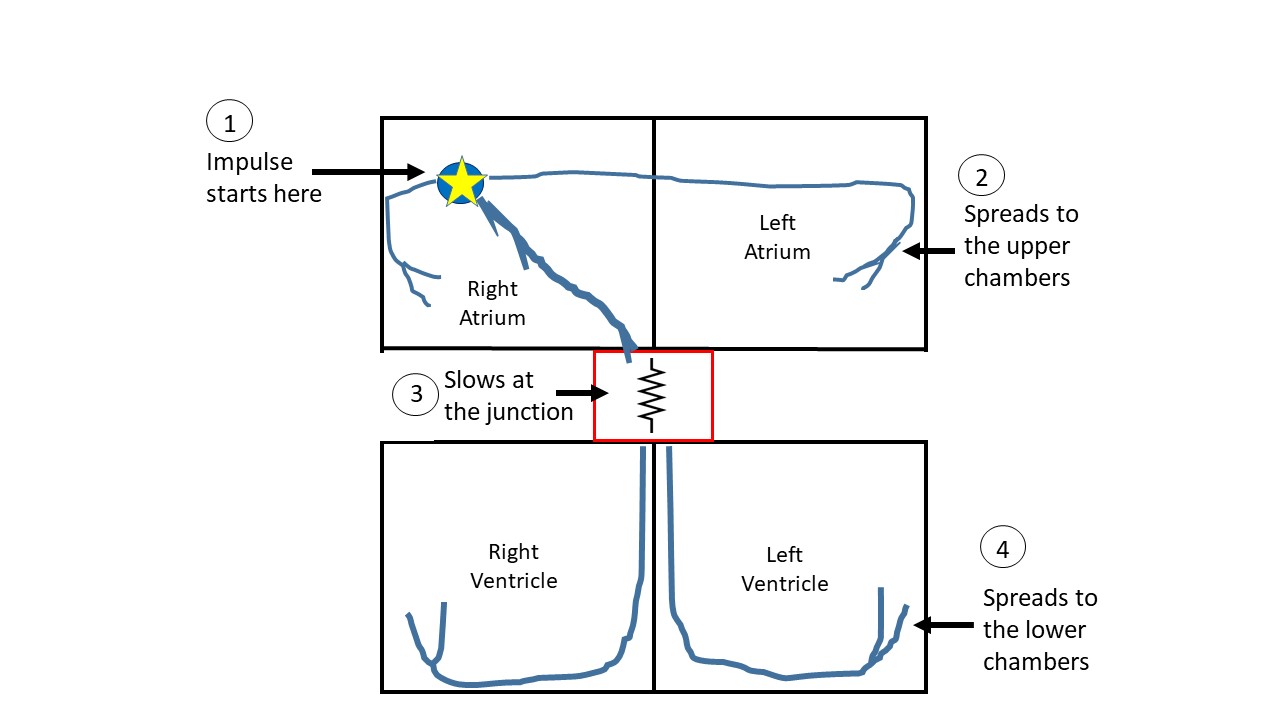
Normally, the electrical impulse for a heart-beat begins in the right upper chamber, at a specialized site called the sinus node. This is a very organized system of electrical wiring explained in the basic anatomy section. If everything goes as per the plan, we have an organized rhythm, like a metronome or a pendulum. The rate of the oscillation may vary but the rhythm remains regular, to and fro (figure 1).
In atrial fibrillation, instead of one single area initiating the impulse in an organized fashion, we have disorganized activity in the upper chambers. Imagine an Olympic sized boat with 40 rowers, listening to a single person in front who is setting the rhythm by shouting ‘Row!’. This is the normal heart. Now imagine various rowers standing up, in no particular order, and shouting ‘Row!’. Other rowers who are not standing up respond to the command, but this results in chaos. The rowers still sticking to their roles of rowing are completely disorganized and also have to paddle more frequently because of the constant commands to do so. This is atrial fibrillation (figure 2).
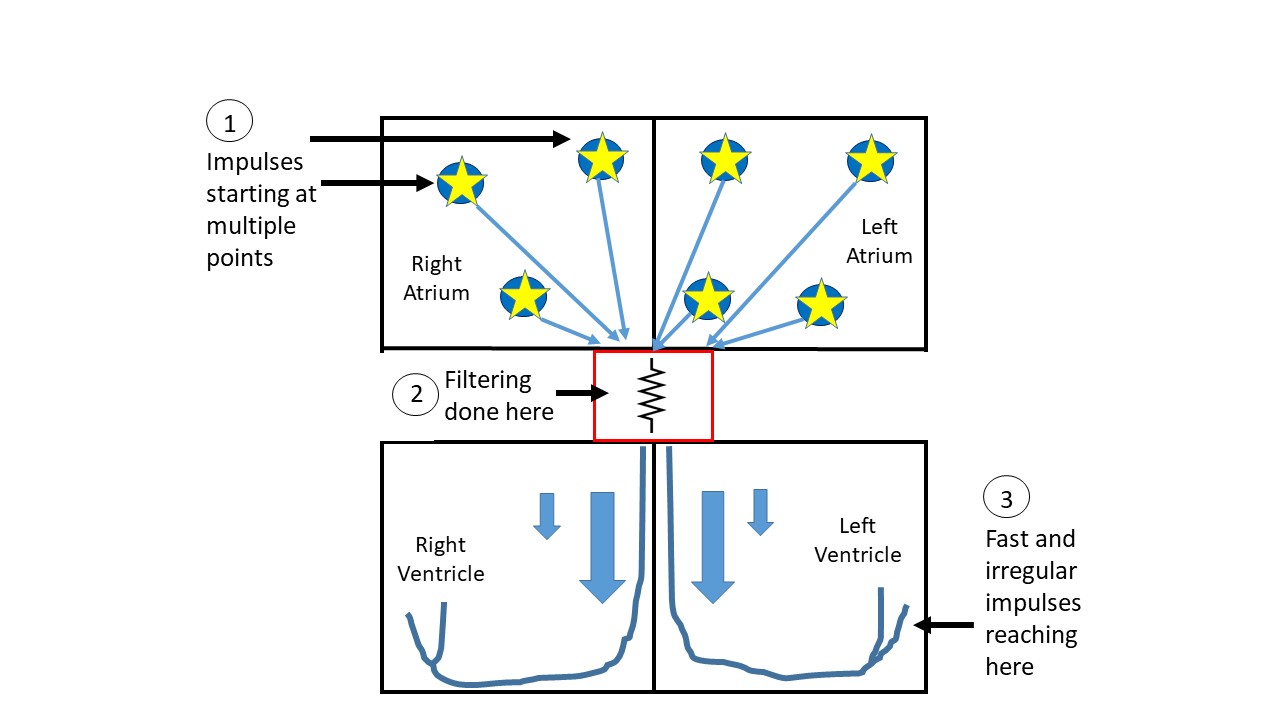
This chaos is happening in both the upper chambers. The electrical impulses may fire as fast as >400 times a minute. If the lower chambers, which have the essential role to pump the blood outside the heart, start going at those rates then this can be fatal. Thankfully, the junction point between the upper and lower chambers (AV node, point#2 in figure 2) functions to filter out excessive impulses. This is because the junction node can only conduct the impulse so many times a minute. It is like the border crossing, irrespective of the number of cars lined up, only so many cars can be processed in a given time and can enter the other country.
Symptoms:
Nevertheless, the lower chambers speed up and may go at a rate of 150-200/minute or more at times. This can be enough to give some people symptoms such as palpitations, shortness of breath, chest pain, dizziness etc. On the other hand, some people may be completely asymptomatic and have no clue they are in atrial fibrillation. The manifestation of the symptoms depends on the effect the fast heart rate has on the body, while some people are excessively sensitive to heart rate change.
While the atrial fibrillation may be permanent, it could also be transient. A big proportion of patients may flip back and forth from normal to atrial fibrillation. This can cause occasional (and unexplained) palpitations, dizziness etc.
People with otherwise normal heart do not miss the lack of contraction of the upper chambers. It is the lower chambers which do the important job of generating enough force to push the blood out of the heart to the body. It is said that the upper chambers may contribute up to 10% to this blood pumping function. Most people have enough reserve to not notice the absence of this 10%. However, patients with poor heart function do not have the luxury of an extra 10% to spare and these patients may especially feel worsening of their symptoms when they go into atrial fibrillation.
Detection:
The only good way to detect atrial fibrillation is to catch it in action. This could be through an ECG, telemetry, holter, event monitor or any other device tracking electrical activity. These devices could also be used to detect the frequency of the flip-flop, back and forth from normal to fibrillation, in diagnosed cases of atrial fibrillation. This condition can also be detected in the hospital by inducing it in a more controlled manner with medications.
What happens if the heart rate of the lower chambers remains fast?:
The heart is not made to run fast all the time. Just like your leg muscles get tired on a treadmill while running, the heart muscles are prone to fatigue if they beat fast all the time. It would be like running a marathon 24 hours a day, 7 days a week. Also, the symptoms become persistent and may worsen with time. In minor proportion of predisposed patients, the rapid electrical activity being supplied to the lower chambers from the upper chambers may trigger automaticity in the lower chambers.
Possibility of stroke:
Going back to the Olympic boat analogy, when the chaos sets in and the rowers are paddling in no particular organization, the movement of the boat is not as effective. Also, the paddlers are rowing too fast to actually dig into the water and push the boat anywhere. The end-result is a complete standstill of the boat. Something similar happens in the upper chambers in atrial fibrillation. The electrical chaos fails to organize an effective contraction of the upper chambers. Consequently, the blood does not move as vigorously through the upper chamber and tends to stagnate in certain cesspools, one of them being an out-pouching of the left upper chamber called the left atrial appendage.
When the blood stagnates, this can result in a blood clot. The risk of forming a clot depends on various risk factors including the age, hypertension, diabetes, previous stroke or heart attack, heart failure, vascular disease and female gender. The more the risk factors, the more the likelihood of clot formation. This blood clot could then be pushed out of the heart and cause a stroke.
Treatment:
The usual approach is to treat the various aspects of atrial fibrillation individually. The rate of the lower chambers is controlled with medications that further slow the junction point (rate control strategy). These medications are usually insufficient in keeping someone in normal rhythm but if atrial fibrillation occurs, they prevent the rate of the lower chambers from going fast. Stroke is prevented through blood thinners and the need for blood thinners is based on the number of risk factors for stroke, as enumerated above.
The question comes in, why not just give medications to prevent atrial fibrillation from occurring in the first place? The answer is related to the efficacy and safety of medications which can do this. Rhythm control medications (which prevent atrial fibrillation from occurring) are not 100% effective. They also have multiple side effects. Some medications can cause automaticity elsewhere in the heart. Most of these medications need constant supervision and monitoring. Some are contraindicated in patients with anatomical heart problems.
The debate for superiority in rate versus rhythm control strategy is ongoing in literature. Most physicians would agree that rate control strategy is better for most patients, largely due to the lack of major side effects. However, in some patients rhythm control strategy works best. These are patients with poor heart function (to preserve the 10% pumping as mentioned above) or severely symptomatic patients, to name a few.
In some cases, medications do not work or cause intolerable symptoms. Under these circumstances, an interventional procedure may be recommended by an Electrophysiologist, who is a cardiologist specializing in the electrical system. Such procedure is called an ablation procedure, involving burning the electrical wiring in the heart. Atrial fibrillation ablation involves burning the circuitry within the upper chambers, along the area of automaticity, electrically isolating them from the rest of the heart. This is like isolating the ‘rogue paddlers’ within a sound-proof bubble so even if they shout instructions to row, no one can hear them. Various studies have claimed good results with the various variants of this procedure. However, most physicians would agree that the result may not be a 100% cure.
Another form of ablation is to burn the junction box (AV node). This is necessary in extreme circumstances, when other attempts have failed and the benefit outweighs the risk. The patient would then have an artificial pacemaker implanted, since the procedure breaks the connection between the natural pacemaker in the right upper chamber to the lower chambers.
The discussion above was to provide a simple understanding of atrial fibrillation management. I would encourage a healthy discussion regarding the risks and benefits of each approach with the cardiologist/electrophysiologist. The discussion is not all-inclusive or exhaustive and individual patient needs may vary.
All opinions expressed here are those of the author and not of the employer. Information provided here is for medical education only. It is not intended as and does not substitute for medical advice.
Podcast of the description:
For video and written description visit: Basics of Atrial Fibrillation page
