Coronavirus (COVID-19) and the heart
The first cases of the novel 2019 coronavirus (COVID-19) was reported in Wuhan, China in December 2019 1 and since has rapidly spread worldwide. In its essence, the virus is a non-living strand of protein called RNA enclosed in a fatty acid envelope.
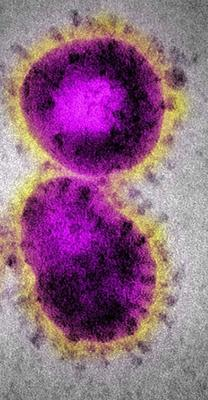
It appears spherical under an electron microscope and has certain particles on its surface which appear like a crown or ‘corona’ (figure 1). Coronavirus can affect the heart in several ways, many of which are still unknown, but the end result is direct injury, heart failure or death.
Why did COVID-19 become such a big deal?
The novel coronavirus has a totally new configuration. Human race has never been exposed to anything like it before, so the entire world population lacks any sort of immunity to this. It seems, every human is susceptible to be infected.
In other words, humans lack antibodies against COVID-19. Antibodies are like special task forces, specialized to disable only one type of foreign cell or protein. These form in the body after an infection or vaccination and prevent future infections with the same organism. Just like the governments around the world are racing to make a vaccine, the human body has its own ‘vaccine lab’ called the plasma cells. Unfortunately, the plasma cells need time while they work on making antibodies. In the meantime, the body sends out its reserve forces against the virus. These soldier cells are not specialized to kill COVID virus and they use any possible means – machine guns, hand grenade, assault tanks against the virus, while the plasma cells can work on making antibodies. In most cases, this is enough to keep the virus suppressed while the antibodies are made. Once the antibodies are ready, the virus is destroyed and the patient recovers after suffering mild symptoms.
In some cases though, the initial response is not enough and the organs (lungs, heart etc.) get caught in this cross-fire between the virus and the soldiers. The result is an overwhelming inflammatory response called a cytokine storm. Cytokines are a byproduct of the war raging inside the infected body. In low levels cytokines help to destroy the virus and only result in mild symptoms like fever. They activate soldier cells all over the body and recruit them to the affected area, like recruiting the military to calm riots inside the country. Cytokines have other favorable functions as well.
However, when the virus levels rise, the war rages on, cytokines build up. Soldier cells all over the body get activated and infiltrate the organs. If the organs are already weak from an underlying disease or old age, they can fail.
Symptoms:
The common symptoms include fever (89% hospitalized patients), cough (68% patients), pain in the throat, headache, tiredness 2. In severe cases it can totally flood the lungs with fluid (pulmonary edema), severely affecting its function. Lungs are like sponge which allow free passage of air, but when soaked in water, no air can pass through. This is called severe acute respiratory distress syndrome or SARS.
For an update on the likely symptoms, refer to the CDC website.
Effect on the heart:
As mentioned above, heart can sustain collateral damage from the cytokines in some cases. There have also been reports of the virus directly injuring heart cells.
Just like the lungs, heart muscle can also get flooded with fluid (myocardial edema) 3 and soldier cells infiltrate the heart. These soldier cells that have been activated by the cytokines are like grenades with pins removed. They destroy the surrounding cells; in this case the heart muscle cells. This is called an inflammation of the heart or myocarditis.
Patients with an underlying heart condition including high blood pressure, heart failure, previous heart attack or heart artery blockages are more susceptible to the above 2. Heart muscle injury is detected by measuring blood levels of a protein called ‘troponin’ which leaks out of dead heart muscle cells. Other such markers in blood, echocardiogram and other imaging techniques can also help diagnose heart damage. Overall, some degree of heart muscle damage can occur in up to 1 in 3 patients 4. Patients who had an underlying heart disease and now have some evidence of heart muscle injury from the virus have the worst death rate (70% in one report 4).
Additionally, the overwhelming cytokine response can also directly affect the blood supply to heart muscles, cause rupture of cholesterol plaques resulting in a heart attack or result in blood clots in various arteries including the heart arteries. These effects are more common in patients with underlying heart artery blockages or previous heart attack 5,6.
How does social distancing work?
Humans as such are widely vulnerable to the virus due to its novel configuration. However, the virus itself is a delicate structure of protein and fat. Left all by itself outside a patient, the virus particle can get damaged by high temperature/heat, dry weather, soap, alcohol and other corrosive agents. The virus cannot maintain itself indefinitely outside a host body (figure 2).
In the absence of vaccination, social distancing is the only possible way to prevent direct contact with the virus particles. Staying at home prevents contact with potential virus-laden spots, while the particles are left outside to ‘die’ (non-living remember?).
All opinions expressed here are those of the author and not of the employer. Information provided here is for medical education only. It is not intended as and does not substitute for medical advice. References are provided at the end of this page. The discussion is not all-inclusive or exhaustive and individual patient findings may vary.
I encourage referring to the CDC website for further information.
.
References:
1. World Health Organization. Pneumonia of unknown cause—China. Accessed January 5, 2020. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/.
2. Guan W-j, Ni Z-y, Hu Y et al. Clinical Characteristics of Coronavirus Disease 2019 in China. New England Journal of Medicine 2020.
3. Inciardi RM, Lupi L, Zaccone G et al. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 2020.
4. Guo T, Fan Y, Chen M et al. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiology 2020.
5. Bonow RO, Fonarow GC, O’Gara PT, Yancy CW. Association of Coronavirus Disease 2019 (COVID-19) With Myocardial Injury and Mortality. JAMA Cardiol 2020.
6. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol 2020.