
Artificial pacemaker for the heart
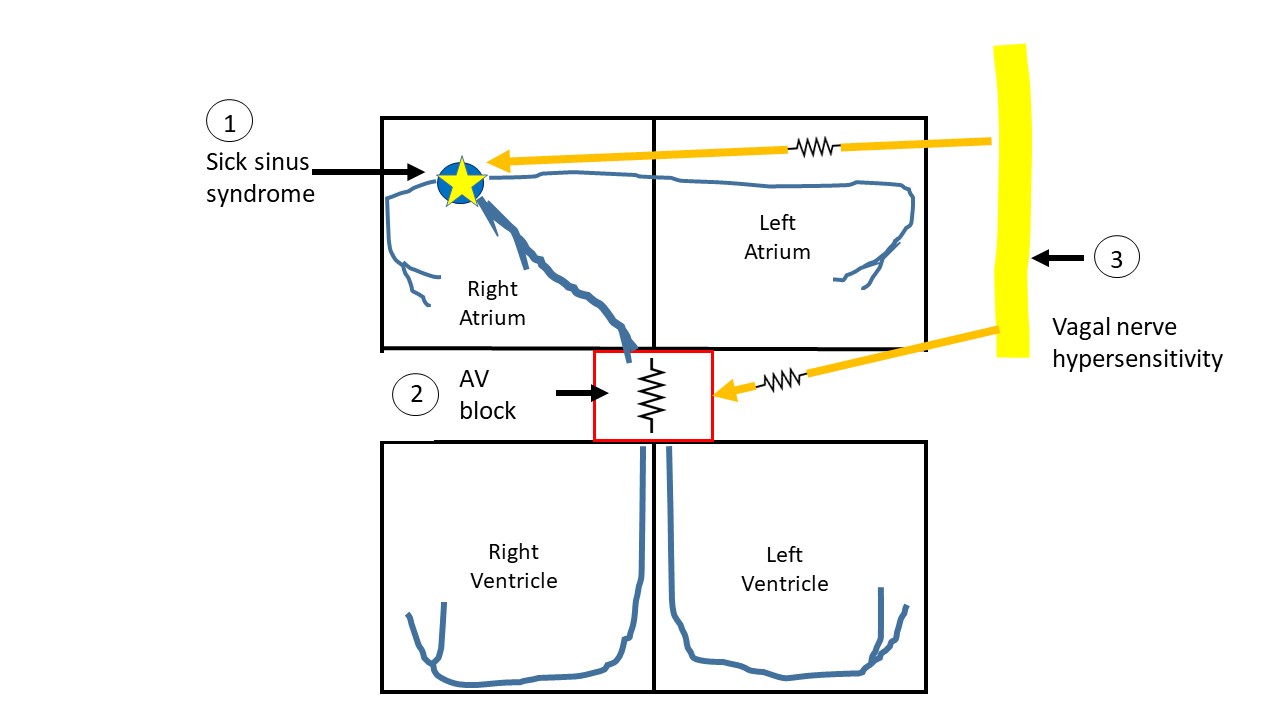
There are conditions when your doctor may inform you that you need a pacemaker. These conditions include sick sinus syndrome when the sinus node (refer to the basic anatomy) loses its ability to set a rhythm, either intermittently or permanently. An artificial pacemaker is needed when the junction box stops conducting or does so slowly or with intermittent failure -> also referred to as AV block. Transient slow heart rate can also be caused by vagal nerve sensitivity with neck movements, straining etc (figure 1). This may be excessive enough to cause loss of consciousness and may need a pacemaker. Under these circumstances the natural electrical system must be supported with an artificial backup.
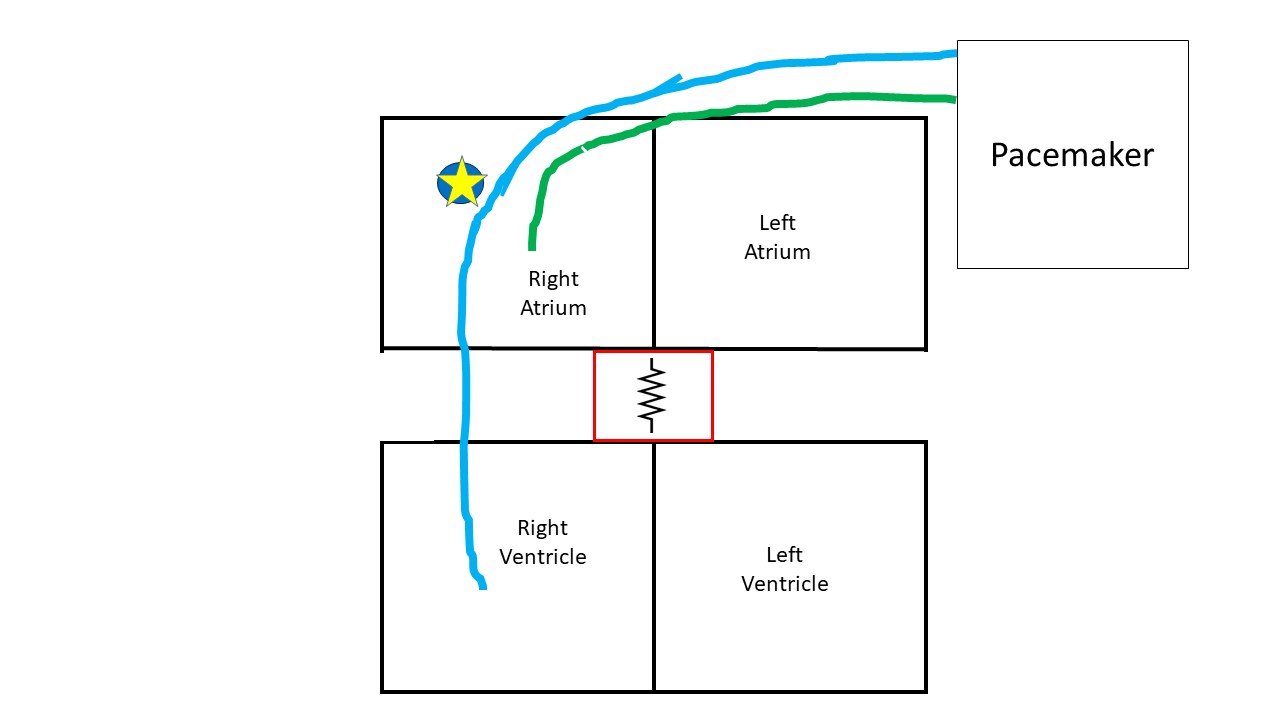
An artificial pacemaker, in its basic form, is a generator implanted over the chest wall, underneath the skin. Wires or leads extend from the generator, enter a vein in the shoulder and travel to the heart. The most common pacemaker sends two leads to the heart (dual chamber). One of the lead goes into the right upper chamber and the second into the right lower chamber (figure 2).
The primary function of the artificial pacemaker is to provide electrical stimulation to the heart when needed. A common misconception is that the artificial pacemaker provides stimulation all the time. This is not always true and depends on the programming of the pacemaker. In fact, the most common settings require the pacemaker to ‘listen’ for native electrical activity and not provide any stimulus if things are working within certain parameters. The pacemaker essentially provides a fail-safe system preventing the heart rate from dropping below a set number. The pacemaker works like a metronome and the cycle is reset every time a heart-beat happens.
The pacemaker also functions as a personal CCTV camera monitoring and recording the heart rhythm all the time. It can be programmed to keep track of heart rhythm or rate fluctuations.
On occasions, it is necessary to have the pacemaker provide stimulation 100% of the time. This runs the risk of draining the battery early. Permanent pacing is needed when a patient needs a higher heart rate than his intrinsic pacemaker to not be symptomatic. If the junction box is non-functional or burned out (as explained in the atrial fibrillation section), then the pacemaker needs to stimulate the right lower chamber all the time. Higher heart rates are needed to prevent a certain rhythm problem called Torsades-de-pointes.
Pacemaker care after placement:
It is recommended to not lift the arm above the head for 2 weeks. A splint may be provided to keep the arm immobilized. This is to prevent the suture site from opening. Some swelling around the pacemaker site immediately after placement is expected, however it is unusual for the swelling to continue growing, appear excessively red, warm, firm or be painful. Drainage or bleeding from the site is also usually abnormal. The pacemaker should be completely underneath the skin and at no point should any part stick out.
MRI compatibility:
Many of the old pacemakers are not FDA-approved to be MRI compatible. Some of the new pacemakers have been tested and approved as MRI-compatible, check with your physician.
On occasions, the pacing leads may be abandoned when removing them is riskier than any benefit. This is especially true for leads placed more than a few months ago, due to scar formation around the leads. In such cases, MRI may cause overheating of these abandoned leads. The presence of abandoned leads should be notified to the physician prior to an MRI.
At the airport:
Inform the TSA officials at the airport of the presence of a pacemaker. A pat-down may be requested.
Prior to a scheduled surgery:
The presence of pacemaker needs to be notified to the surgeon. The surgeon may consult with the company representative, who may ask for a visit before and/or after the surgery to check the pacemaker.
Troubleshooting:
If the pacemaker makes noise, this needs to get checked. It usually signifies that the battery is up for renewal, but there are other conditions when it may make a noise. During the battery replacement procedure, the generator on the chest wall is swapped with a new one. It is essential to get the pacemaker checked at least once a year
Drainage or infection may require the pacemaker to be removed completely.
Three chamber pacemakers:
Certain conditions need a pacemaker which also stimulates the left lower chamber. This involves a third lead. This is usually necessary in advanced heart pump failure to maintain synchronized pumping of the lower chambers.
Some facts:
The pacemaker does not prevent the heart from going fast. It only prevents it from going slower than a programmed number.
The pacemaker cannot shock the heart. This would need a defibrillator.
Electrical stimulation provided by a dual chamber pacemaker to the heart are not felt.
There are exceptions to everything!
Understand what is a defibrillator here.
Follow on twitter.
All opinions expressed here are those of the author and not of the employer. Information provided here is for medical education only. It is not intended as and does not substitute for medical advice.
